Background:
Sickle cell disease (SCD) patients have a higher risk of maternal and neonatal morbidity during pregnancy than the general population. Pregnancy in SCD is associated with increased metabolic demands, a hypercoagulable state, endothelial dysfunction, severe anemia, and increased vaso-occlusive episodes. We designed a study to retrospectively review the clinical outcomes of pregnant patients with SCD and SCD trait to examine the incidence of maternal and perinatal morbidity and mortality. We hypothesized that SCD patients should have a higher morbidity during pregnancy and SCD trait patients should not have higher morbidity.
Methods:
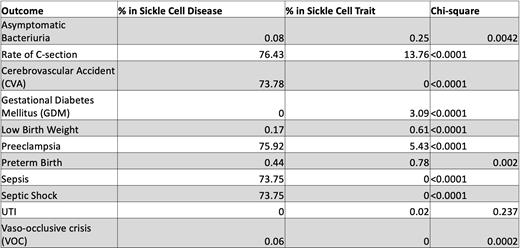
We conducted a retrospective cohort study and reviewed 29,822 patient encounters. Pregnant patients with the SCD genotype - Hb SS, Hb S beta 0 thalassemia, Hb S beta + thalassemia and Hb SC disease, and sickle cell trait (SCD trait) - Hb AS were included. Maternal clinical outcome variables for the entire pregnancy duration were vaso-occlusive crisis (VOC), deep vein thrombosis (DVT), pulmonary embolism (PE), infections - sepsis, septic shock, asymptomatic bacteriuria, acute pyelonephritis, and urinary tract infection (UTI), cerebrovascular accident (CVA), myocardial infarction (MI) and transient ischemic attack (TIA). Clinical outcome variables for pregnancy complications were preeclampsia, gestational diabetes mellitus (GDM), and C-section rate. Clinical outcome variables for neonatal complications included preterm birth and low birth weight. ICD 9 and ICD 10 codes were used to search for the pregnancy, SCD, sickle cell trait, maternal and neonatal outcomes. Data was collected from the Health Facts Database, which contains de-identified information from electronic medical records (EMR) of hospitals in which Cerner© has a data use agreement. The categorical clinical outcome variables were analyzed using Chi-square test.
Results:
There were 29,822 patient encounters reviewed. Patients with SCD had higher percentages for C-section rates, CVA, preeclampsia, sepsis, septic shock, and VOC compared to those with SCD trait. C-section rates were higher in SCD patients with 76.43% versus 13.76% in SCD trait patients. CVA was higher in SCD patients with 73.78% versus 0% in SCD trait patients. Preeclampsia was higher in SCD patients with 75.92% in SCD patients versus 5.43% in SCD trait patients. Sepsis and septic shock were higher in SCD patients with 73.75% in SCD patients versus 0% in SCD trait patients. VOC was evident in SCD patients with 0.06% versus 0% in SCD trait patients. Patients with SCD trait had higher percentages for asymptomatic bacteriuria, GDM, low birth weight, preterm birth, and UTI compared to patients with SCD. Asymptomatic bacteriuria was higher in SCD trait patients with 0.25% versus 0.08 in SCD patients. GDM was higher in SCD trait patients with 3.09% versus 0% in SCD patients. Low birth weight was higher in SCD trait patients with 0.61% versus 0.17% in SCD patients. Preterm birth was higher in SCD trait patients with 0.78% versus 0.44% in SCD patients. UTI was noted in SCD trait patients with 0.02% versus 0% in SCD patients. There were no findings for DVT, PE, acute pyelonephritis, MI, and TIA in both SCD and SCD trait patients.
Conclusion:
Pregnant patients with SCD were more likely to have C-sections, CVA, preeclampsia, sepsis, septic shock, and VOC. Pregnant patients with SCD trait were more likely to have asymptomatic bacteriuria, GDM, low birth weight, preterm birth, and UTI. Our findings indicate that prevention and management of CVA, preeclampsia, sepsis, and septic shock is important for pregnant patients with SCD to prevent adverse maternal and neonatal outcomes. The higher rate of C-sections may have been to reduce the severity of maternal and perinatal morbidity in SCD patients. Our study has significant limitations - retrospective nature and use of ICD9 and ICD10 codes for clinical outcome variables. Certain clinical outcome variables, such as CVA, sepsis or septic shock, may have been overestimated as these diagnoses may have been recorded prior to the start of pregnancy in the EMR. Nevertheless, SCD patients have higher maternal and perinatal morbidity that needs to be addressed.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal